Enhanced PhilHealth Benefits Packages For COVID-19 Patients
3 min readThe Philippine Health Insurance Corporation (Philhealth) has enhanced its package benefits for its members and dependents amid the spread of COVID-19. This is to help affected Filipinos with their hospitalization expenses.

These are the enhanced PhilHealth benefits packages for COVID-19 patients you should know:
1. ER & Tent admission coverage
With cases at an all-time high and hospitals experiencing a surge in COVID-19 related admissions, PhilHealth has assured patients that those who are admitted in emergency rooms and tents within hospital compound pending availability of rooms will be covered.
In a new advisory released by PhilHealth:
patients, including those battling the coronavirus disease 2019 (Covid-19), admitted and managed in the ER due to lack of rooms, shall receive full benefits if the stay is at least 24 hours
2. Free COVID-19 test
PhilHealth benefits shall include the free COVID-19 Test as a response to the increasing number of Patients Under Investigation (PUI). According to Proclamation No. 922, the public health emergency response package is on top of the quarantine packages and referral packages.
The benefit means that every person with a suspected case of the viral disease can go through the health examination without any fees to pay.
To note, the initial COVID test kits used are imported and expensive, but the University of the Philippines’ National Institute of Health has created a local test kit at a much lower price. Since the samples are approved by the FDA, they will be used for mass testing starting April 4.
3. Referral Package
An individual who has been declared a PUI must be transferred from a first-level hospital to a healthcare facility that has more capability for the isolation procedure and the handling of infectious disease. This benefit is called the Referral Package that a PhilHealth member can avail of.
The benefit amount will be used for the hospital bill of the member for the initial management, stabilization, and proper transfer of the member-patient to a higher-level medical facility.
Amount of benefit: P4,000
(Read: List Of Drugstores With Delivery Services)
4. Isolation Package
PhilHealth members who are mild and asymptomatic that need to undergo quarantine/isolation due to COVID-19 can avail of this isolation benefit package.
Known as the “COVID-19 Home Isolation Package” (CHIBP). this circular applies to:
“all claims for home isolation services filled by accredited PhilHealth isolation facilities, infirmaries, hospitals and Konsulta providers who have accomplished the necessary documentary requirements to provide the CHIBP,”
To be eligible for CHIBP, you must meet the social and critical criteria for home quarantine and are able to receive health support directly from your home.
PhilHealth said that only accredited facilities in areas identified as “surge areas” by the inter-agency task force on COVID-19 (IATF) can apply for re-accreditation as CHIBP providers until December this year. Patients covered by CHIBP should also be living in areas identified as high-risk.
Surge areas, as defined by PhilHealth, are those high-risk geographic areas declared by the IATF.
Corresponding reimbursement rate: P5,917 per claim.
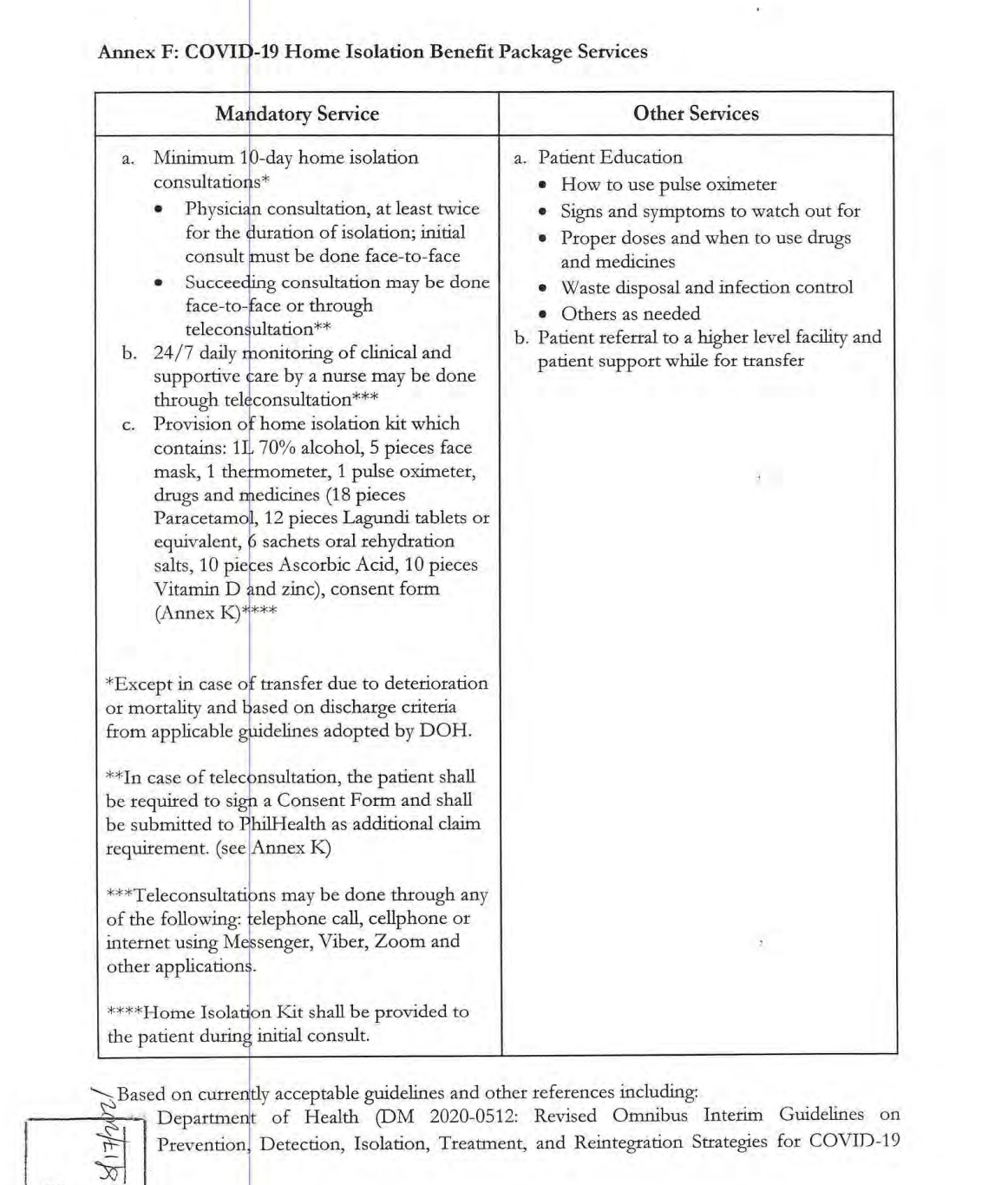
These are the services covered by CHIBP:
5. Existing Case Rate Package
If you are a COVID-positive patient diagnosed with other diseases like pneumonia (because of the causative agent such as the novel coronavirus) can take advantage of the PhilHealth packages for existing medical case rates.
Amount of benefit per disease:
- Mild pneumonia: P43,997
- Moderate pneumonia: P143,267
- Severe pneumonia: P333,519
- Critical pneumonia: P786,385
The intermediate package for previously managed as probable Covid-19 case but had negative reverse transcription-polymerase chain reaction test results are also covered amounting to PHP18,000 and PHP38,000 for moderate and severe/critical pneumonia, respectively.
6. No Balance Billing
No Balance Billing Policy is another PhilHealth benefit for patients who are old and indigent. This means that after confinement in public hospitals, the exceeding bill from their PhilHealth coverage for COVID-19 will be waived.
How to file claims for COVID-19 PhilHealth benefits
Claimants must submit the following documents to the medical facility before the patient gets discharged:
- COVID-19 tests and results (photocopy)
- PhilHealth Claim Signature Form (filled out and signed)
- PhilHealth Claim Forms 1, 2, and 4 (filled out and signed)
- Statement of Account
- PhilHealth Membership Registration Form (for non-members)
Do you have further questions about the COVID-19 coverage from PhilHealth? It’s best to get in touch with PhilHealth via their official contacts:
- Action Center hotline: 8441-7442
- Mobile SMS: 0917898-74442
- Facebook account: @PhilHealthofficial
- Twitter account: @teamphilhealth
- Email address: actioncenter@philhealth.gov.ph
Update: Article originally posted April 2020. Information has been updated as of the current data available.
